Baby Sleep Basics: Guide for New Parents | Sleepgram
Share
Baby Sleep Basics for New Parents

Navigating the Dreamy (and Not-So-Dreamy) World of Baby Sleep
Welcoming a new baby into the family is a time of immense joy, profound love, and, often, overwhelming exhaustion. As new parents embark on this beautiful journey, questions and anxieties surrounding their baby's sleep are incredibly common and entirely normal.1 The well-worn phrase "sleep like a baby" often conjures images of peaceful, uninterrupted slumber. However, the reality for many new parents is quite different. Newborns, while they do sleep a significant portion of the day, do so in short, unpredictable bursts, frequently waking for nourishment and comfort.1 This discrepancy between the popular idiom and the actual sleep patterns of a young infant can be a source of stress and self-doubt. Understanding the true nature of baby sleep from the outset can help set realistic expectations and alleviate some of this common parental anxiety.
Sleep is not merely a passive state for infants; it is a period of intense activity and crucial for their rapid growth and development. During sleep, a baby's brain is hard at work, forming new connections, consolidating memories, and supporting the maturation of the nervous system.5 Adequate sleep is also fundamental for their physical growth and overall well-being.8 Furthermore, when a baby sleeps better, it allows parents the opportunity for much-needed rest, which is vital for their own health, patience, and ability to navigate the demands of caring for a newborn.1
This guide aims to offer clear, gentle, and evidence-based information to help new parents understand their baby's evolving sleep needs from the newborn stage through the first year. It will explore typical sleep patterns, provide guidance on establishing calming bedtime routines, and detail the essential safe sleep practices designed to protect little ones. The focus is on education and empowerment, providing practical strategies without promoting specific products, all delivered with an understanding and supportive voice.
Understanding Your Newborn's Sleep (0-3 Months): The First Chapter of Rest
The first three months of a baby's life are characterized by rapid changes, and sleep is no exception. Understanding the unique nature of newborn sleep is the first step towards navigating this period with confidence.
How Much Sleep Do Newborns Really Need?
Newborns spend a large portion of their day sleeping, typically totaling around 14 to 17 hours within a 24-hour period according to recommendations from the National Sleep Foundation and the American Academy of Sleep Medicine 8, with some sources indicating up to 16 to 18 hours.1 It is important to remember that this is an average, and just like adults, individual babies will have slightly different sleep needs.3
This substantial amount of sleep doesn't usually happen in long, consolidated stretches. Instead, newborns sleep in short bursts, often lasting from 20 to 50 minutes 3 or 1 to 2 hours at a time 4, though some naps may extend to 2 to 4 hours.1 These frequent wakings are biologically driven. Newborns have tiny stomachs and need to feed frequently, typically every 2 to 3 hours, to support their rapid growth and development.9 This pattern of fragmented sleep due to essential feeding needs is a normal and expected part of the newborn phase, not an indication of a "bad" sleeper or a reflection of parenting.
The erratic sleep seen in newborns is a direct consequence of their physiological immaturity and their fundamental needs for nourishment and growth. Attempts to impose a rigid sleep schedule too early are unlikely to succeed and can create unnecessary stress for both the baby and the parents. The focus during these early months should be on responsive care, meeting the baby's needs as they arise, while gently guiding them towards a more predictable rhythm over time.
Decoding Newborn Sleep Cycles: Active vs. Quiet Sleep
Newborn sleep is not just one uniform state. It is characterized by two main types of sleep: "active sleep" and "quiet sleep".3
-
Active Sleep: This is similar to REM (Rapid Eye Movement) sleep in adults. During active sleep, a baby might move their arms and legs, make little grunting or sighing sounds, twitch, grimace, or even open their eyes briefly. Their breathing can also be irregular during this phase. Newborns spend a considerable amount of their sleep time in this active state.4 It's easy for parents to mistake these movements and sounds for signs that the baby is waking up, but often they are still asleep.
-
Quiet Sleep: This is more akin to non-REM sleep. In quiet sleep, the baby lies relatively still, their breathing is deeper and more regular, and they are less likely to move or make sounds.
Newborn sleep cycles, which include both active and quiet sleep, are much shorter than adult sleep cycles, typically lasting around 20 to 50 minutes.3 It is perfectly normal for babies to wake briefly or stir between these sleep cycles before, hopefully, settling back to sleep. Understanding these distinct sleep states and the nature of their sleep cycles can help parents avoid intervening unnecessarily when their baby is simply transitioning between cycles or is in a period of active sleep. A moment of observation can often reveal that the baby will settle back down on their own.
Day and Night, All Mixed Up: Helping Your Baby Learn the Difference
One of the most common challenges for new parents is that their newborn seems to have their days and nights reversed, sleeping soundly during the day and being more wakeful at night. This is because newborns do not yet have an established internal body clock, or circadian rhythm, and their bodies are not yet producing the sleep hormone melatonin in a regular day-night pattern.3 They simply don't distinguish between daytime and nighttime in the way adults do.3
While this will develop naturally over time, parents can gently help their baby learn the difference between day and night with a few simple strategies:
-
During the day: Expose the baby to natural daylight by opening curtains or spending time in well-lit rooms. Maintain normal household noise levels and engage in gentle play and interaction when the baby is awake.3 There's no need to tiptoe around a napping newborn during the day; getting them used to some ambient noise can be beneficial.12
-
At nighttime: Create a calm, soothing sleep environment. Keep the lights dim, even during feedings and diaper changes. Minimize interaction and keep voices soft and quiet.3 The goal is to make nighttime less stimulating and more conducive to sleep.
These gentle cues, consistently applied, can support the baby's natural development of a day-night rhythm. It's about guiding this process, not forcing it.
Why So Many Wakings? The Role of Hunger, Comfort, and Communication
As mentioned, the primary reason for a newborn's frequent wakings is their need for regular feedings to fuel their rapid growth.1 However, hunger isn't the only reason a baby might wake and cry.
Crying is a newborn's primary way of communicating their needs.3 They might cry because they:
-
Are hungry
-
Have a wet or soiled diaper
-
Are too hot or too cold
-
Feel uncomfortable
-
Need to be burped
-
Simply want comfort and closeness
It's also important for parents to be aware that many newborns go through a period of increased crying, sometimes referred to as "purple crying" or the "witching hour," which is often most intense in the late afternoon and evening. This phase typically starts around 2 weeks of age, peaks around 6-8 weeks, and gradually subsides by 3-4 months.3 During these times, a baby may cry for no apparent reason and can be difficult to soothe.
Understanding that frequent waking and crying are normal developmental phases and the baby's way of communicating can help parents respond with patience and empathy, rather than feeling that something is wrong or that they are failing to meet their baby's needs.
A particularly interesting aspect of newborn wakefulness is the "quiet alert phase".15 When a newborn first wakes, before hunger cues typically escalate to crying, there is often a period where the baby is calm, still, and attentively taking in their surroundings, responding to sounds and motion. Crying, in contrast, is often a late sign of hunger, and a baby who has reached a state of distress may be too upset to feed effectively.15 Recognizing and responding during this quiet alert phase offers a valuable window for calm connection, gentle interaction, and initiating a feeding before the baby becomes distressed. This proactive approach can lead to calmer feeding experiences and potentially make it easier for the baby to settle back to sleep, reframing some waking moments not just as "sleep interruptions" but as opportunities for positive engagement.
"I'm Sleepy!" – Recognizing Your Newborn's Tired Cues
Learning to recognize when a newborn is tired, even before they become fussy or start crying, is a key skill for parents. Responding to these early "sleepy cues" can make it much easier to settle a baby for a nap or bedtime, as an overtired baby often has more difficulty falling asleep and staying asleep.6
Common tired signs in newborns include 3:
-
Rubbing eyes
-
Yawning (this can be a late cue for some babies)
-
Looking away or avoiding eye contact
-
Fussing or becoming more irritable
-
Making jerky movements with arms or legs
-
Developing a glazed or unfocused look in their eyes
-
Clenching fists
-
Making soft, whimpering, or "sleepy" sounds
By becoming attuned to their individual baby's specific tired cues, parents can act as "baby detectives," helping to ensure their little one gets the rest they need when they need it, preventing the cycle of overtiredness that can make sleep more challenging for everyone.
Navigating Infant Sleep (4-12 Months): New Patterns Emerge
As babies grow beyond the initial newborn stage, their sleep patterns begin to mature and change significantly. This period, from roughly 4 to 12 months, often brings longer stretches of nighttime sleep and more predictable nap schedules, though it also comes with its own set of developments and potential disruptions.
The Sleep Shift: Longer Nights, Consolidated Naps
Around the 3 to 6-month mark, many parents will notice a welcome shift in their baby's sleep. Many babies start sleeping for longer continuous periods at night. For example, some may sleep for 4 to 6 hour stretches 1, while others might manage 5 hours 5 or even 6 to 8 hours without waking.4 By the time they are 6 months old, about two-thirds of babies are able to sleep through a significant portion of the night.1
Daytime naps also tend to become more predictable and consolidated during this phase. The 3 or 4 (or more) short, scattered naps of the newborn period often transition into 2 or 3 more regular naps of longer duration.7 This evolution is partly due to the maturation of the baby's circadian rhythm and more regular melatonin production, which is typically better established by about 3 months of age.7 This developmental progression offers hope to tired parents that the intense, round-the-clock care of the newborn phase does indeed evolve.
How Much Sleep Do Infants Need? (Ages 4-11 Months)
As infants grow, their total sleep needs gradually decrease, but they still require a substantial amount of sleep for healthy development. For infants aged 4 to 11 months, guidelines from the National Sleep Foundation suggest 12 to 15 hours of sleep per 24-hour period.8 The American Academy of Sleep Medicine recommends a similar range of 12 to 16 hours for infants aged 4 to 12 months, inclusive of naps.8
The following table provides a general overview of typical sleep needs, breaking them down further within the first year. It's important to view these as general guidelines, as every baby is an individual.
|
Age Range |
Total Sleep (in 24 hrs) |
Typical Nighttime Sleep |
Typical Daytime Naps (Number & Approx. Duration) |
Sources |
|
0-1 Month |
14-18 hours |
8-10 hours (interrupted) |
6-8 hours (multiple short naps, 1-2 hrs each) |
1 |
|
1-3 Months |
14-17 hours |
8-10 hours (interrupted) |
4-7 hours (3-5 naps, varying lengths) |
3 |
|
4-6 Months |
12-16 hours |
10-12 hours (may still wake for 1-2 feeds) |
3-5 hours (2-3 naps, 30 mins - 2 hrs each) |
4 |
|
6-9 Months |
12-16 hours |
10-12 hours (may sleep through or wake for 0-1 feed) |
2-4 hours (2 naps, 1-2 hrs each; some may take a 3rd short nap) |
4 |
|
9-12 Months |
12-15 hours |
10-11 hours (often sleeps through) |
2-4 hours (usually 2 naps, 1-2 hrs each) |
4 |
Note: These are general ranges. Individual baby sleep needs can vary. Always observe a baby's cues and consult with a healthcare provider if there are concerns.
While these figures offer a useful benchmark, it's crucial to remember that they are just guidelines. A baby's mood, energy levels, and overall well-being when awake are often better indicators of whether they are getting sufficient rest than strictly adhering to a chart.11 If a baby is generally happy, alert, and developing well, they are likely getting the sleep they need, even if it doesn't perfectly match the averages.
Understanding Wake Windows: The Sweet Spot for Sleep
A "wake window" refers to the amount of time a baby can comfortably and happily stay awake between periods of sleep (e.g., between one nap and the next, or between the last nap and bedtime). Understanding and respecting a baby's optimal wake window is a practical tool that can significantly help with settling them for sleep.7
Putting a baby down for sleep within their ideal wake window—not too soon when they aren't tired enough, and not too late when they've become overtired—can lead to easier settling and better quality sleep. An overtired baby often has more difficulty falling asleep and may sleep more restlessly.
General wake window guidelines by age are:
-
4-6 months: Approximately 1.5 to 2.5 hours 9
-
6-9 months: Approximately 2 to 3.5 hours 9
-
9-12 months: Approximately 2.5 to 4 hours 9
Observing a baby's tired cues (discussed earlier) in conjunction with these general wake window timings can help parents find that "sweet spot" for sleep, reducing guesswork and potentially preventing some sleep struggles.
Developmental Detours: When Milestones Meet Sleep (Sleep Regressions)
Just when parents feel they might have their baby's sleep figured out, a "sleep regression" can occur. These are periods when a baby who was previously sleeping relatively well suddenly starts waking more frequently at night, having trouble settling for naps or bedtime, or resisting sleep altogether.6
These disruptions often coincide with significant developmental milestones, such as learning to roll over, sit up, crawl, or stand. Teething, growth spurts, and cognitive leaps like developing object permanence (the understanding that things and people still exist even when out of sight) can also temporarily throw sleep off track.6 Common ages for these so-called regressions include around 4 months, 6 months, and 8-10 months.6
The brain is working overtime during these periods of intense learning and physical development, which can make it harder for a baby to settle down or stay asleep. They might even seem eager to practice their new skills in the crib! For instance, the development of object permanence around 8-10 months can lead to increased separation anxiety, as the baby now understands that when a parent leaves the room, they haven't disappeared but have gone somewhere else, prompting them to call out or resist being left alone.
It's reassuring for parents to know that these sleep disruptions are usually temporary and are often a positive sign of their baby's healthy growth and development.6 Sleep development isn't always a straight, linear path; there will be ups and downs. During these phases, maintaining consistency with established calming routines as much as possible can provide an anchor for the baby and help them return to more settled sleep patterns once the developmental leap has been integrated.7
As babies approach the 4-month mark and beyond, their ability to form associations becomes much stronger.11 This is a significant developmental step, but it also means that how a baby falls asleep can become a more ingrained habit. If a baby consistently relies on external help to fall asleep—such as being rocked, fed, or held until they are fully asleep—these can become "sleep onset associations".1 When they naturally wake between sleep cycles during the night 3, they may be unable to return to sleep on their own without that specific association being replicated. These babies are sometimes referred to as "signalers" because they signal or cry out for parental help to get back to sleep.18 This developmental shift in associative learning makes the 4-6 month period a pivotal time. It can either solidify dependent sleep habits or, with gentle encouragement, foster more independent sleep skills. This underscores why practices like establishing a consistent bedtime routine and aiming for the "drowsy but awake" approach become increasingly important as an infant grows.
Crafting a Calming Bedtime Routine: Your Gentle Blueprint
A consistent and calming bedtime routine is one of the most effective tools parents have for promoting healthy sleep habits in their baby. It’s more than just a series of steps; it’s a predictable and comforting ritual that signals to a baby that it's time to wind down and prepare for sleep.
The Magic of Consistency: Why Routines Matter
A predictable sequence of calming activities performed each evening helps a baby's internal clock to regulate and signals to their body and mind that sleep is approaching.1 This consistency can make bedtime a smoother, less stressful experience for both baby and parents, often reducing fussiness and helping the baby fall asleep more easily and potentially sleep for longer periods.1
Beyond the practical benefits for sleep, bedtime routines offer a wonderful opportunity for dedicated one-on-one time and connection between parent and child. These quiet moments of interaction build positive sleep associations and strengthen the parent-child bond. The predictability of a routine creates a sense of security for the baby, helping them feel safe and relaxed. For parents, especially new parents navigating a period of immense change, a routine can provide a comforting sense of structure and a proactive way to nurture their baby's well-being. The emotional benefits of these shared rituals—the bonding, the shared calm, the reduction in anxiety for both parent and child—are just as significant as the sleep-inducing ones.
When to Begin? Starting Simple and Soothing
Parents can begin to introduce elements of a simple, soothing routine very early on, even in the newborn phase.26 However, it's important to distinguish this from formal "sleep training," which is generally not appropriate for newborns.6 A more intentional and consistent bedtime routine can typically be established around 6 to 8 weeks of age 6, or as parents start to observe more predictable patterns in their baby's day.
The key is to start simply. The routine doesn't need to be long or elaborate, especially in the beginning.22 Even a short sequence of 2-3 calming activities can be effective. This gentle entry point reassures parents that they don't need a complex plan from day one but can gradually build and adapt the routine as their baby grows.
Gentle Bedtime Routine Ideas: Creating Calm and Connection
The most effective bedtime routines consist of 3-4 calming activities performed in the same order each night to create predictability.24 The specific activities can be tailored to the family's preferences and the baby's temperament, but the focus should always be on calm and connection. Here are some ideas (none of which require specific products):
-
A Warm Bath: A soothing bath can be very relaxing for a baby. The subsequent cooling of the body temperature after a warm bath can also naturally help trigger sleepiness.23 This can be a lovely, calming part of the routine.4
-
Gentle Massage: After a bath, or as a standalone activity, a few minutes of gentle massage with a baby-safe, unscented lotion or oil can promote relaxation and is a wonderful way to bond.6
-
Dressing for Sleep: Changing into comfortable pajamas and a fresh diaper signals a transition. For babies who are no longer swaddled, a wearable blanket or sleep sack (ensuring it is not weighted28) can provide a sense of security and warmth.22
-
Quiet Feeding: For many babies, a final feeding (breast or bottle) is a comforting part of the wind-down process.6 If feeding to sleep becomes a strong association that disrupts later sleep, parents might consider moving the feed slightly earlier in the routine.
-
Reading a Story or Singing a Lullaby: The sound of a parent's calm voice reading a short story or singing a gentle lullaby is incredibly soothing for a baby. This also promotes language development and provides a special moment of closeness.1
-
A Final Cuddle and Goodnight Phrase: A consistent goodnight kiss, cuddle, and a soft, loving phrase (e.g., "Goodnight, sweet baby, I love you") can be the final cue that it's time for sleep.14
It's important to avoid stimulating activities, loud noises, and screen time (TV, phones, tablets) in the hour or so leading up to bedtime, as these can make it harder for a baby to wind down and fall asleep.1
The "Drowsy But Awake" Approach: A Gentle Nudge to Independent Sleep
A cornerstone of gentle sleep guidance is the "drowsy but awake" technique. This involves putting the baby into their crib or bassinet when they are clearly sleepy and ready for bed, but not yet fully asleep.1
The reason this approach is so often recommended is that it gives the baby the opportunity to associate their own sleep space with the process of falling asleep. It allows them to practice the skill of settling themselves to sleep, which is crucial for being able to fall back asleep independently if they wake during the night.1
This technique can be introduced gradually after the very early newborn period. Some experts suggest around 3 months of age 26, while others note it can be attempted with careful observation even earlier.10 The key is that it's an opportunity, not a rigid rule that must cause distress. Success with "drowsy but awake" is highly dependent on accurately recognizing the baby's tired cues and timing it right. An overtired baby put down awake will likely struggle much more than a baby who is perfectly drowsy. It's a delicate balance, a bit like walking a tightrope, requiring parents to be attuned to their baby's signals. If it causes significant upset, parents might need to offer more comfort initially, perhaps by patting or shushing the baby in the crib, and gradually reduce their intervention over time. It’s about finding the balance that works for that individual baby at that particular moment, emphasizing gentle guidance rather than a one-size-fits-all mandate.
Creating a Sleep Sanctuary: The Ideal Sleep Environment
The environment where a baby sleeps plays a significant role in how easily they fall asleep and how well they stay asleep. Optimizing the sleep space helps to remove external barriers to sleep and reinforces the cues that it's time to rest.
-
Darkness: A dark room signals to the brain that it's time for sleep. Using blackout curtains or blinds can be very helpful, especially for daytime naps or during summer months when it stays light later in the evening.2
-
Quiet: While newborns can often sleep through some household noise, a generally quiet environment is conducive to sleep as they get older. Some babies are soothed by continuous, low-level white noise, like the hum of a fan or a white noise machine (though no specific products are endorsed here). The key is a consistent sound that masks other, more disruptive household noises.6
-
Cool Temperature: Babies sleep best in a room that is cool but comfortable. A general guideline is a temperature that would be comfortable for a lightly clothed adult, often cited as between 68-72°F (20-22°C).6 Overheating should be avoided.
-
Safety: Above all, the sleep environment must be safe. This means adhering strictly to all safe sleep guidelines, which will be detailed in the next section.
Safe Sleep Essentials: Protecting Your Precious Little One

Ensuring a safe sleep environment for a baby is one of the most critical responsibilities of new parenthood. The following guidelines are based on recommendations from leading pediatric health organizations, such as the American Academy of Pediatrics (AAP), and are designed to significantly reduce the risk of Sudden Infant Death Syndrome (SIDS) and other sleep-related infant deaths. These practices are non-negotiable for every sleep, both at night and for naps.
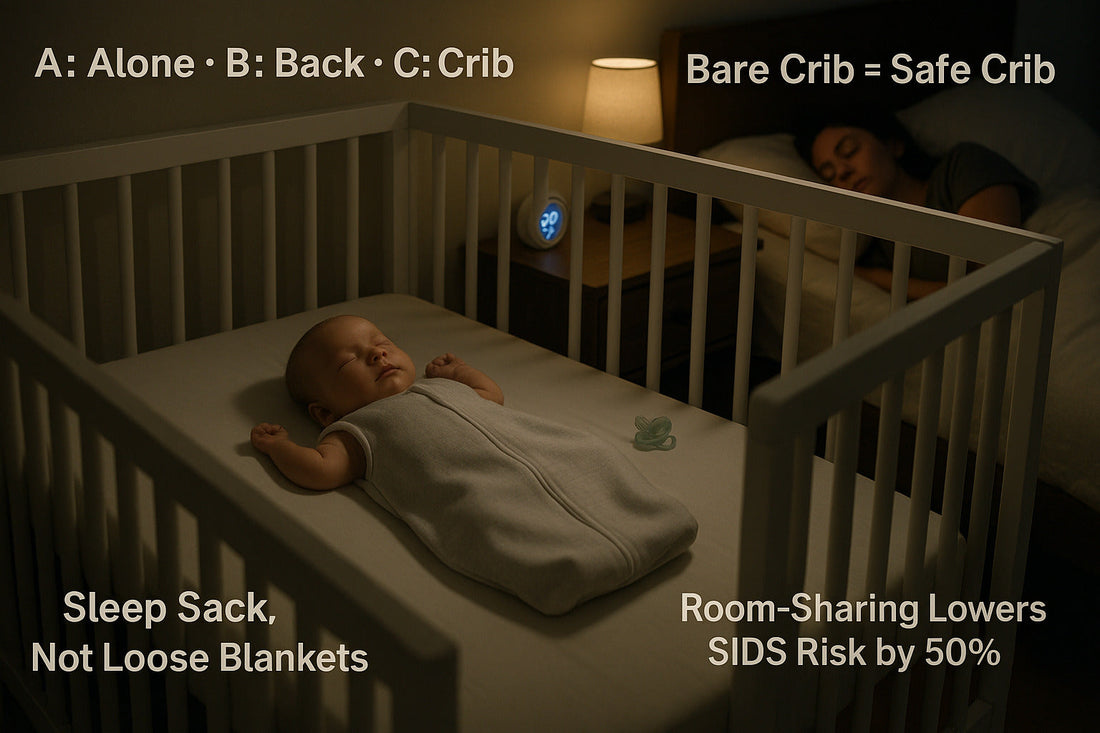
The ABCs of Safe Sleep: The Golden Rules
A simple way to remember the core tenets of safe sleep is the ABCs:
-
Alone: Your baby should sleep alone in their own designated sleep space.
-
Back: Always place your baby on their back to sleep.
-
Crib: Your baby should sleep in a safety-approved crib, bassinet, or portable play yard. 2
These ABCs should be followed for every sleep, whether it's for a short nap during the day or for nighttime sleep, and by every caregiver.2
Back to Sleep: Why It's a Lifesaver
Placing a baby on their back for every sleep is one of the most effective actions parents can take to lower the risk of SIDS.2 Some parents worry that their baby might choke if they spit up while lying on their back, but a baby's anatomy and their gag reflex naturally help to prevent choking, even in this position.28 In fact, babies who sleep on their backs are much less likely to die of SIDS than babies who sleep on their stomachs or sides.
Once a baby can consistently roll from their back to their stomach and also from their stomach back to their back on their own, they can usually be allowed to find their own preferred sleep position. However, it is still crucial to always place them on their back at the beginning of every sleep period.2
The Ideal Sleep Surface: Firm, Flat, and Fitted
The surface where a baby sleeps must be:
-
Firm: It should not indent when the baby is lying on it. A firm mattress in a safety-approved crib, bassinet, or portable play yard is recommended.2
-
Flat: The sleep surface should not be at an angle or inclined.
-
Covered only by a fitted sheet: No other bedding should be used on the mattress.
Soft surfaces like adult beds, sofas, armchairs, waterbeds, or piles of pillows are dangerous for infant sleep. These surfaces increase the risk of suffocation (if the baby's face presses into the soft material) and entrapment (if the baby gets wedged between a mattress and a wall, or in couch cushions).5 Similarly, products that are not specifically marketed and safety-tested for infant sleep, such as Boppy pillows, Dock-a-Tots, or other in-bed sleepers, should not be used for unsupervised sleep.34 If a baby falls asleep in a car seat, stroller, swing, or infant carrier, they should be moved to a firm, flat sleep surface as soon as it is safe and practical to do so.34
Keep the Crib Bare: Nothing But Baby (and a Fitted Sheet!)
A safe crib is a bare crib. The only thing in the crib with the baby should be a firm mattress covered by a tightly fitted sheet.2
This means NO:
-
Loose blankets
-
Pillows (of any size or shape)
-
Comforters or quilts
-
Stuffed animals or soft toys
-
Crib bumpers (padded or mesh) or related products that attach to crib slats or sides
These items, while often marketed as comfort or decorative items, pose serious risks of suffocation, entrapment, or strangulation.10 Many well-intentioned parents add these items to make the crib seem "cozier" or to prevent minor bumps, but the risks far outweigh any perceived benefits. If parents are concerned about their baby being cold, a wearable blanket (also known as a sleep sack) is a safe alternative to loose blankets. It is important to ensure that any wearable blanket used is not weighted, as weighted products are not safe for infants.11
The following checklist summarizes the key do's and don'ts for a safe sleep environment:
|
Feature |
Safe (DO) |
Unsafe (AVOID) |
|
Sleep Position |
Always place baby on their BACK for every sleep. |
Placing baby on stomach or side to sleep. |
|
Sleep Surface |
Use a FIRM, FLAT mattress in a safety-approved crib, bassinet, or play yard. Covered only by a fitted sheet. |
Soft surfaces (adult beds, sofas, armchairs, pillows), inclined sleepers, surfaces not designed for infant sleep. |
|
Bedding |
Use only a FITTED SHEET designed for the mattress. Consider a wearable blanket (sleep sack) for warmth if needed (not weighted). |
Loose blankets, quilts, comforters, sheepskins, mattress toppers. |
|
Crib Items |
Keep the crib BARE. |
Pillows, stuffed toys, crib bumpers (all types), wedges, positioners, loose items of any kind. |
|
Sleep Location |
Baby sleeps ALONE in their own crib/bassinet/play yard in the SAME ROOM as parents for at least 6 months. |
Bed-sharing (baby in adult bed), sleeping on a couch or armchair with baby, baby sleeping in a room alone (for first 6-12 months). |
|
Temperature |
Dress baby in light sleep clothing; room comfortable for a lightly clothed adult. AVOID OVERHEATING. |
Over-bundling baby, covering baby's head with hats indoors (after hospital). |
|
Clothing/Swaddle |
If swaddling, ensure it's not too tight, allows hip movement, and stop when baby shows signs of rolling. |
Swaddling too tightly, swaddling once baby can roll, weighted swaddles/sleepers. Pacifier cords or attachments to clothing. |
|
Environment |
SMOKE-FREE environment. |
Smoking near baby or in baby's home. |
Based on recommendations from sources including.2
Understanding the "why" behind these rules can empower parents to make the safest choices. For example, soft bedding can conform to a baby's face and obstruct their airway, increasing the risk of suffocation or rebreathing exhaled air (carbon dioxide), which is a factor in SIDS.10 Back sleeping helps keep the airway clear. This knowledge transforms parents from simply following rules to becoming active protectors of their infant, better equipped to resist outdated advice or misleading marketing.
Room-Sharing, Not Bed-Sharing: Keeping Baby Close and Safe
The American Academy of Pediatrics recommends that babies sleep in their parents' room, close to the parents' bed, but on a separate, safe sleep surface (such as a crib, bassinet, or portable play yard) for at least the first 6 months of life, and ideally up to one year.1
This practice of room-sharing (baby in the same room, but not the same bed) has several benefits:
-
It can decrease the risk of SIDS by as much as 50%.1
-
It makes it easier for parents to feed, comfort, and monitor their baby during the night.
It is crucial to distinguish room-sharing from bed-sharing. Bed-sharing, where the baby sleeps in the adult bed with parents or other children, is not recommended due to significant safety risks, including 1:
-
Suffocation from soft adult bedding (pillows, comforters).
-
Overlay (an adult accidentally rolling onto the baby).
-
Entrapment (baby getting trapped between the mattress and bed frame, headboard, or wall).
The risks of bed-sharing are even higher if:
-
The parent smokes or the mother smoked during pregnancy.
-
The parent has consumed alcohol, medications that cause drowsiness, or illicit drugs.
-
The baby is younger than 4 months old.
-
The baby was born prematurely or with a low birth weight.
-
The sleep surface is soft, or there is soft bedding present. 34
Despite clear guidelines, unsafe sleep practices, including bed-sharing or using soft bedding, persist.29 Parental decisions are complex and influenced by many factors beyond just medical knowledge, including cultural norms, family traditions, persuasive marketing of non-essential baby products, and strong emotional desires, such as wanting the baby to feel "cozy" with blankets or wanting to bed-share for bonding or ease of feeding.33 It is important to acknowledge these emotional pulls and practical considerations with empathy, while gently but firmly redirecting towards the safest options. Room-sharing offers the closeness many parents desire without the risks of bed-sharing, and wearable blankets provide warmth without the dangers of loose bedding.
Temperature Check: Not Too Hot, Not Too Cold
Babies should be dressed lightly for sleep. A general rule of thumb is to dress the baby in no more than one additional layer than what an adult would wear to be comfortable in the same room environment.2
Overheating can increase the risk of SIDS, so it's important to ensure the baby doesn't get too hot.2 Parents can check if their baby is too warm by feeling their chest or back; if it feels sweaty, the baby is likely too hot. It's also important to avoid covering the baby's head with hats or hoods indoors once they are home from the hospital, as this can also lead to overheating.2
Other Important Safety Considerations
Beyond the ABCs and crib environment, several other factors contribute to a safer sleep experience for infants:
-
Smoke-Free Environment: Exposure to tobacco smoke, both during pregnancy and after birth, significantly increases the risk of SIDS. Babies should always be in a completely smoke-free environment.1
-
Breastfeeding: Breastfeeding is associated with a reduced risk of SIDS. If possible, breastfeeding is encouraged.30
-
Pacifier Use: Offering a clean, dry pacifier at nap time and bedtime may help reduce the risk of SIDS. If breastfeeding, it's often recommended to wait until breastfeeding is well-established (usually a few weeks) before introducing a pacifier. The pacifier should not be attached to the baby's clothing or any other object with a string or clip, as this poses a strangulation risk.1
-
Avoid Alcohol and Illicit Drug Use: Parents and caregivers should avoid alcohol and illicit drug use, as these substances can impair their awareness and ability to care for the baby safely, especially if bed-sharing occurs.31
A Gentle Note on "Sleep Training": Understanding Foundations First
The term "sleep training" is widely discussed among parents, and it often brings to mind various methods aimed at helping a baby learn to fall asleep independently and self-soothe if they wake during the night.6
It is important for new parents to understand that formal "sleep training" methods, particularly those that involve leaving a baby to cry for extended periods, are generally not recommended for newborns or very young infants (typically before 4 to 6 months of age).6 Newborns have strong needs for responsive care, frequent feedings, and comfort. Their sleep patterns are still developing, and they are not yet developmentally ready for more structured sleep interventions.
This guide focuses on establishing healthy sleep foundations from the earliest days. These foundations include understanding a baby's evolving sleep patterns, creating consistent and calming bedtime routines, ensuring a meticulously safe sleep environment, and responding to a baby's needs with sensitivity and warmth. These are the prerequisites for healthy sleep, regardless of any approaches parents might consider later on.
Practices such as putting a baby down "drowsy but awake" and implementing consistent, soothing bedtime routines are gentle ways to encourage independent sleep skills over time, without the distress that can be associated with some formal training methods.1 These early, gentle approaches can be thought of as "sleep shaping"—guiding a baby toward healthy habits from an early age by creating positive associations with sleep and providing opportunities for them to develop self-settling skills. This distinction can help parents feel empowered to positively influence their baby's sleep from the very beginning, without feeling pressured to engage in more intensive "training" methods before their baby, or they themselves, are ready. These early efforts in laying a healthy foundation are invaluable and align with a gentle approach to parenting.
Parental Well-being: Taking Care of Yourself Through the Haze of Sleeplessness
The arrival of a new baby brings immense joy, but it also brings significant changes to a parent's life, most notably to their sleep. The focus is naturally on the baby's needs, but parental well-being is equally crucial during this demanding time.
The Unspoken Challenge: Parental Sleep Deprivation
A baby's sleep patterns, especially in the early months, have a profound impact on their parents' ability to get adequate rest. Frequent night wakings for feeding, changing, and comforting can lead to significant sleep deprivation for parents, affecting their mood, energy levels, cognitive function, and overall ability to cope.1 Feelings of exhaustion, frustration, and overwhelm are common and valid experiences for new parents.1
The connection between parental sleep and baby sleep is strong. A tired, stressed parent may find it more challenging to remain patient and consistent with bedtime routines or to respond calmly to their baby's night wakings. Conversely, when a baby begins to sleep for longer stretches, it allows parents to get more rest, which in turn improves their resilience and coping capacity. Supporting parental rest is, therefore, an indirect way of supporting the baby's sleep journey.
Gentle Strategies for Your Own Rest
While uninterrupted nights of sleep may be a distant dream in the early stages, there are strategies parents can use to maximize their own rest:
-
Sleep when the baby sleeps: This age-old advice still holds true. Even short naps during the day when the baby is sleeping can help to recharge energy levels. It might be tempting to use that time for chores, but prioritizing rest is often more beneficial.1
-
Share nighttime duties: If there is a partner, working as a team can make a significant difference. Divide responsibilities for nighttime feedings (if bottle-feeding or using expressed breast milk), diaper changes, and settling the baby. This allows each parent to get at least some consolidated blocks of sleep.1
-
Prioritize rest over household chores: The house does not need to be perfect. During these demanding early months, it's okay to let some chores slide in favor of catching up on sleep.1
-
Practice good sleep hygiene for yourself: As much as possible, try to create a restful sleep environment for yourself. This includes minimizing caffeine intake, especially in the afternoon and evening, and reducing exposure to screens (phones, tablets, TV) before bed, as the blue light can interfere with sleep.1
The Power of Support: Asking for and Accepting Help
New parents should not feel they have to do everything on their own. Building a support system and learning to ask for and accept help is vital.
-
Lean on partners, family, and friends: Don't be hesitant to ask for practical help. This could be a family member watching the baby while a parent naps, a friend bringing over a meal, or help with household tasks.1
-
Utilize parental leave: If available, taking advantage of parental leave policies can provide dedicated time to focus on the baby and adjust to new routines, which can also facilitate more opportunities for rest.1
Remembering that needing help is not a sign of weakness but a normal part of the parenting journey can make it easier to reach out and build a supportive village.
Conclusion: Embracing the Journey with Patience, Confidence, and Love
Navigating the world of baby sleep can feel like a complex puzzle, especially for new parents who are also adjusting to so many other changes. However, by understanding the fundamental principles of infant sleep, parents can approach this aspect of their journey with greater confidence and calm.
The key messages to carry forward are:
-
Understand Your Baby's Development: Recognize that newborn and infant sleep patterns are driven by their developmental stage and individual needs. What is normal for a one-month-old is different from what is typical for a six-month-old.
-
Embrace Gentle Routines: Consistent, calming bedtime routines are powerful tools for signaling sleep and creating positive associations. These rituals also offer precious moments of connection.
-
Prioritize Safe Sleep, Always: The guidelines for safe sleep are paramount and non-negotiable. A safe sleep environment protects a baby from preventable risks and provides peace of mind for parents.
-
Practice Patience and Self-Compassion: There will be good nights and challenging nights. Progress is not always linear. Be patient with the baby and, just as importantly, with oneself.
This journey of guiding a child towards healthy sleep habits is one that unfolds over time. Things do generally get easier as babies mature and develop more predictable sleep rhythms.1 Trust in the process, celebrate the small victories, and remember that providing a loving, responsive, and safe environment is what matters most.
If at any point there are persistent concerns about a baby's sleep, development, or a parent's own well-being and ability to cope, it is always advisable to consult with a trusted healthcare provider, such as a pediatrician or family doctor. They can offer personalized guidance and support.2 With knowledge, support, and a gentle approach, new parents can successfully navigate the sleepy world of their little ones.
Works cited
-
New Parents: Tips for Quality Rest | Johns Hopkins Medicine, accessed May 27, 2025, https://www.hopkinsmedicine.org/health/wellness-and-prevention/new-parents-tips-for-quality-rest
-
Baby sleep | UNICEF Parenting, accessed May 27, 2025, https://www.unicef.org/parenting/child-care/baby-sleep
-
Typical sleep behaviour (1) – newborns 0 to 3 months | Better Health ..., accessed May 27, 2025, https://www.betterhealth.vic.gov.au/health/healthyliving/typical-sleep-behaviour-nb-0-3-months
-
Infant Sleep - Stanford Medicine Children's Health, accessed May 27, 2025, https://www.stanfordchildrens.org/en/topic/default?id=infant-sleep-90-P02237
-
Helping baby sleep through the night - Mayo Clinic, accessed May 27, 2025, https://www.mayoclinic.org/healthy-lifestyle/infant-and-toddler-health/in-depth/baby-sleep/art-20045014
-
Newborn Sleep Guide: How Many Hours, Baby Noises & More, accessed May 27, 2025, https://www.whattoexpect.com/first-year/newborn-sleep.aspx
-
Developmental Leaps In Babies - Smart Sleep Coach by Pampers™, accessed May 27, 2025, https://www.smartsleepcoach.com/blog/sleep-problems/how-developmental-milestones-can-impact-your-babys-sleep
-
Youth screen media habits and sleep: sleep-friendly screen ..., accessed May 27, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC5839336/
-
How Much Do Babies Sleep? A First Year Baby Sleep Schedule - Happiest Baby, accessed May 27, 2025, https://www.happiestbaby.com/blogs/baby/first-year-sleep-schedule
-
Newborn Sleep Schedules: What to Expect From 0 to 3 Months, accessed May 27, 2025, https://www.parents.com/baby/sleep/basics/understanding-baby-sleep-1-3-months/
-
Baby Sleep Questions, Answered | Children's Hospital of Philadelphia, accessed May 27, 2025, https://www.chop.edu/news/health-tip/baby-sleep-questions-answered
-
Helping your baby to sleep - NHS, accessed May 27, 2025, https://www.nhs.uk/baby/caring-for-a-newborn/helping-your-baby-to-sleep/
-
How to Set Good Sleep Patterns for Your Baby - WebMD, accessed May 27, 2025, https://www.webmd.com/parenting/baby/newborns
-
Sleep 0 – 3 months - Healthy WA, accessed May 27, 2025, https://www.healthywa.wa.gov.au/Articles/S_T/Sleep-0-3-months
-
Newborn Sleep Patterns | Johns Hopkins Medicine, accessed May 27, 2025, https://www.hopkinsmedicine.org/health/wellness-and-prevention/newborn-sleep-patterns
-
Sleep Patterns: Babies, 4-12 Months | Happy Baby Organics, accessed May 27, 2025, https://www.happyfamilyorganics.com/learning-center/article/sleep-patterns-for-a-baby-ages-4-12-months/
-
Newborn to Toddler: Helping Your Baby Sleep – Good Start Canada, accessed May 27, 2025, https://goodstartbaby.ca/blogs/articles/newborn-to-toddler-helping-your-baby-sleep
-
Sleep in Infants (2-12 Months) - Nationwide Children's Hospital, accessed May 27, 2025, https://www.nationwidechildrens.org/specialties/sleep-disorder-center/sleep-in-infants
-
Infant sleep routine – Easy ideas for Early Years practitioners | A Unique Child, accessed May 27, 2025, https://www.teachearlyyears.com/a-unique-child/view/easy-ways-to-encourage-healthy-sleep-in-nursery
-
www.betterhealth.vic.gov.au, accessed May 27, 2025, https://www.betterhealth.vic.gov.au/health/healthyliving/typical-sleep-behaviour-nb-0-3-months#:~:text=Newborns%20generally%20sleep%2012%20to,20%20to%2050%20minutes%20long.
-
How to get your baby to nap longer - BabyCenter, accessed May 27, 2025, https://www.babycenter.com/baby/sleep/how-can-i-get-my-baby-to-nap-longer_7695
-
How To Establish A Baby Bedtime Routine - Love to Dream, accessed May 27, 2025, https://lovetodream.com/blogs/baby-sleep/night-time-routine
-
Setting Your Baby's Bedtime Routine - Cleveland Clinic Health Essentials, accessed May 27, 2025, https://health.clevelandclinic.org/bedtime-routine-for-babies
-
Newborn Bedtime Routine for Baby: The Complete Guide - Nested Bean, accessed May 27, 2025, https://www.nestedbean.com/blogs/zen-blog/newborn-bedtime-routine
-
www.heavensentsleep.com, accessed May 27, 2025, https://www.heavensentsleep.com/blog/how-bedtime-routine-evolves-with-age#:~:text=As%20they%20grow%20out%20of,20%20minutes%20(after%20feeding).
-
8 Questions on Creating Sleep Routines | Nanit, accessed May 27, 2025, https://www.nanit.com/blogs/parent-confidently/ama-questions-on-sleep-routines
-
Articles – tagged "Parenting Tips" - Good Start Canada, accessed May 27, 2025, https://goodstartbaby.ca/blogs/articles/tagged/parenting-tips
-
Helping Babies Sleep Safely | Reproductive Health - CDC, accessed May 27, 2025, https://www.cdc.gov/reproductive-health/features/babies-sleep.html
-
Safe baby sleep: What parents need to know | Norton Children's ..., accessed May 27, 2025, https://nortonchildrens.com/news/baby-really-sleep-room/
-
Safe Sleep - AAP, accessed May 27, 2025, https://www.aap.org/en/patient-care/safe-sleep/
-
Providing Care for Babies to Sleep Safely | SUID and SIDS | CDC, accessed May 27, 2025, https://www.cdc.gov/sudden-infant-death/sleep-safely/index.html
-
safe infant sleeping: Topics by Science.gov, accessed May 27, 2025, https://www.science.gov/topicpages/s/safe+infant+sleeping.html
-
Safe Baby Sleep Practices | Raleigh Infant CPR Classes, accessed May 27, 2025, https://cpreducatorsinc.com/safe-baby-sleep-practices-to-reduce-sids/
-
Updated SIDS prevention recommendations from the AAP: - Piedmont Pediatrics, accessed May 27, 2025, https://www.piedmontpediatrics.net/updated-american-academy-of-pediatrics-sudden-infant-death-syndrome-prevention-recommendations
-
safesleep.mo.gov, accessed May 27, 2025, https://safesleep.mo.gov/american-academy-of-pediatrics-recommendations/#:~:text=Avoid%20use%20of%20soft%20bedding,as%20much%20as%2050%20percent.
Parent Decision-Making and How to Influence Decisions - ResearchGate, accessed May 27, 2025, https://www.researchgate.net/publication/390611338_Parent_Decision-Making_and_How_to_Influence_Decisions
