Better Sleep During Menopause | Sleepgram
Share
Navigating Night Sweats & Sleepless Nights: Your Guide to Better Sleep During Menopause

Menopause is a significant life transition, and for many, it brings a host of changes, not least of which is the quality of sleep. If you've found yourself tossing and turning, battling night sweats, or simply unable to drift off like you used to, you're far from alone. In fact, a 2024 survey by the American Academy of Sleep Medicine revealed that 50% of women aged 45-64 report that menopause sometimes, often, or always disrupts their sleep.
Understanding why these changes occur and learning how to cope can make a world of difference. At Sleepgram, we believe that quality rest is foundational to well-being at every stage of life. This guide will explore the common sleep challenges during menopause, the role of hormonal shifts, and practical strategies—including cooling sleep tips—to help you reclaim restful nights.
Why Does Menopause Affect Sleep? The Hormonal Connection
The primary culprits behind menopausal sleep disturbances are fluctuating and declining hormone levels, particularly estrogen and progesterone. These hormones play crucial roles in regulating various bodily functions, including sleep.
-
Estrogen's Role: Estrogen is involved in the metabolism of serotonin and other neurotransmitters that affect our sleep-wake cycle. It helps regulate body temperature, which is vital for sleep onset and maintenance. As estrogen levels decline, this can lead to several sleep-disrupting symptoms. The North American Menopause Society (NAMS) notes that these hormonal shifts are a key reason for increased sleep problems.
-
Progesterone's Impact: Progesterone has a natural calming and sleep-promoting effect. It stimulates GABA receptors in the brain, which helps reduce anxiety and can have a slightly sedative effect. As progesterone levels fall during perimenopause and menopause, this can contribute to difficulty sleeping, increased anxiety, and a reduced ability to cope with stress.
-
Melatonin Changes: Melatonin, the primary hormone that regulates the sleep-wake cycle, also tends to decrease with age, and menopause can further affect its levels, potentially contributing to sleep problems.
These hormonal shifts don't just make it harder to fall asleep; they can also lead to more frequent awakenings and a decrease in deep, restorative sleep.
Common Sleep Stealers During Menopause
Several specific symptoms and conditions linked to menopause can wreak havoc on your sleep:
Hot Flashes and Night Sweats
Perhaps the most notorious menopause symptom, hot flashes (and their nighttime counterpart, night sweats) affect a significant number of women. Up to 75% of women in perimenopause experience them. A hot flash is a sudden feeling of intense warmth, often accompanied by sweating and a rapid heartbeat, which can be incredibly disruptive to sleep. Research shows that awakenings can even precede the hot flash itself, triggered by changes in the brain.
Coping & Cooling Tips:
-
Dress Lightly: Opt for lightweight, breathable cotton pajamas and use cotton bed linens. The cotton sheets or cooling Sleepgram bamboo sheets can be excellent choices.
-
Cool Your Bedroom: Keep your bedroom temperature cool, ideally around 18 degrees Celsius (65 degrees Fahrenheit). Use fans or air conditioning to improve air circulation.
-
Bedding Strategies: Use light covers instead of heavy blankets. Consider a cooling gel pillow or putting a cold pack under your pillow, and flip your pillow to the cool side when you feel warm. A comfortable, breathable Sleepgram comforter can also make a difference.
-
Avoid Triggers: Be mindful of foods and drinks that can trigger hot flashes, such as spicy foods, caffeine, and alcohol, especially before bed.
-
Cool Drinks: Keep a glass of cold water by your bed to sip if you wake up feeling warm.
-
Layer Clothing: Dress in layers that you can easily remove if a hot flash strikes.
Insomnia
Insomnia—difficulty falling asleep, staying asleep, or waking too early—is very common during menopause, with over 60% of postmenopausal women reporting insomnia symptoms. This can be a direct result of hormonal changes or exacerbated by other symptoms like hot flashes and anxiety.
Managing Insomnia:
-
Consistent Sleep Schedule: Go to bed and wake up at the same time each day, even on weekends, to regulate your body's internal clock.
-
Relaxation Routine: Establish a calming pre-sleep routine. This could include reading, taking a warm bath, listening to soothing music, or practicing gentle yoga or meditation.
-
Limit Screen Time: Avoid blue light from phones, tablets, and TVs at least an hour before bed, as it can interfere with melatonin production.
-
Cognitive Behavioral Therapy for Insomnia (CBT-I): This type of therapy has been shown to be effective for menopausal insomnia by helping to change thoughts and behaviors around sleep. If you can't sleep, get out of bed after 15-20 minutes and do something quiet and non-stimulating until you feel sleepy again.
-
Optimize Your Pillow: Ensure your pillow is providing the right support and comfort. An adjustable pillow like the Sleepgram luxe adjustable pillow can be tailored to your needs.
Anxiety and Mood Swings
The hormonal shifts of menopause can also contribute to increased anxiety, irritability, and mood swings, all of which can make it difficult to relax and fall asleep.
Coping Strategies:
-
Stress Management: Practice stress-reducing techniques like deep breathing, meditation, or yoga.
-
Regular Exercise: Physical activity can help improve mood and reduce anxiety, but avoid vigorous exercise close to bedtime.
-
Seek Support: Talk to friends, family, or a therapist if anxiety or low mood is significantly impacting your life.
Sleep-Disordered Breathing (including Sleep Apnea)
Postmenopausal women are two to three times more likely to develop sleep apnea compared to premenopausal women. This condition involves repeated pauses in breathing during sleep, often accompanied by snoring, and can lead to fragmented sleep and daytime fatigue. The decline in estrogen and progesterone may contribute to changes in body fat distribution and airway collapsibility, increasing the risk.
What to Do:
-
If you or your partner notice loud snoring, gasping, or pauses in breathing during sleep, consult your doctor. They may recommend a sleep study.
-
Maintaining a healthy weight and avoiding alcohol before bed can also be helpful.
Restless Legs Syndrome (RLS)
RLS is characterized by an uncomfortable urge to move the legs, often worse in the evenings and at night, making it difficult to fall asleep. It's more common in women and can become more prevalent or severe during perimenopause and menopause. Fluctuating estrogen levels and their potential impact on dopamine (a neurotransmitter involved in muscle movement) may play a role. Iron deficiency, which can occur with heavy perimenopausal bleeding, is also linked to RLS.
Easing RLS:
-
Movement & Massage: Gentle stretching, walking, or massaging your legs before bed may help.
-
Hot/Cold Therapy: Applying a hot compress or taking a warm bath can be soothing.
-
Iron Check: If you suspect iron deficiency, ask your doctor for a blood test. Iron supplements may be beneficial if levels are low.
-
Avoid Caffeine: Limiting caffeine intake, especially in the evening, is advisable.
Lifestyle Adjustments for Better Menopausal Sleep

Beyond addressing specific symptoms, several lifestyle changes can promote better sleep quality during menopause:
-
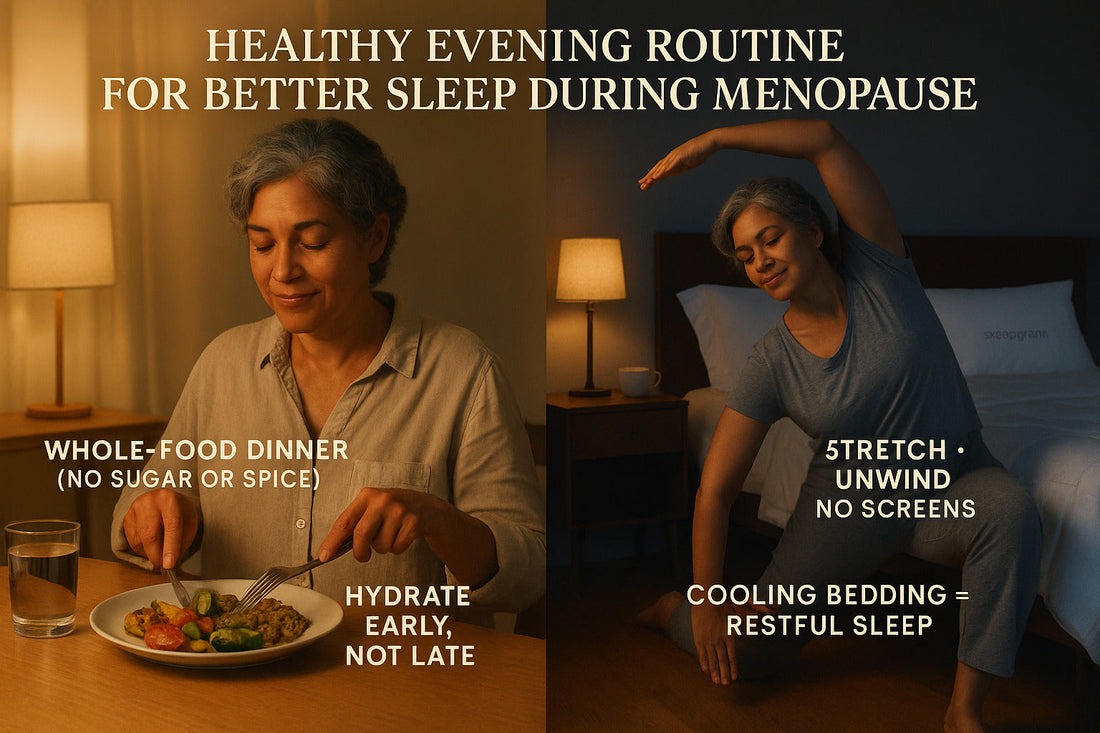
Healthy Diet: Eat a balanced diet rich in fruits, vegetables, and whole grains. Avoid heavy meals, spicy foods, and excessive sugar, especially close to bedtime.
-
Regular Exercise: Aim for regular physical activity, but try to finish workouts at least a few hours before bed. Weight-bearing exercises are also important for bone health.
-
Limit Caffeine and Alcohol: Both can interfere with sleep and may worsen hot flashes. Avoid them in the late afternoon and evening.
-
Quit Smoking: Nicotine is a stimulant and can negatively impact sleep. Smoking is also linked to an increased risk of hot flashes.
-
Hydration Timing: Drink plenty of fluids during the day but reduce intake in the hours leading up to bedtime to minimize nighttime bathroom trips.
-
Comfortable Sleep Environment: Beyond temperature, ensure your bedroom is dark and quiet. A comfortable mattress and supportive pillows are key. Consider a Sleepgram mattress protector to keep your mattress fresh. The right pillowcase, like a smooth Sleepgram pillowcase or a luxurious Sleepgram silk pillowcase, can also enhance comfort.
When to Seek Medical Advice
While many sleep issues can be managed with lifestyle changes, it's important to talk to your doctor if:
-
Sleep problems are persistent and significantly impacting your quality of life.
-
You suspect you might have a sleep disorder like sleep apnea or severe RLS.
-
You're struggling with anxiety or depression.
Your doctor can discuss various treatment options, which may include hormone therapy (HT) for some women, non-hormonal medications, or referral to a sleep specialist or therapist. HT can be effective for managing hot flashes and improving sleep for some, but it's a decision to be made carefully with your healthcare provider.
Embracing Restful Nights Through Menopause
Menopause might bring changes to your sleep, but it doesn't have to mean an end to restful nights. By understanding the underlying causes, implementing targeted coping strategies for symptoms like hot flashes, and adopting healthy sleep habits, you can navigate this transition with greater comfort and wake up feeling more refreshed.
Prioritizing your sleep is an investment in your overall health and well-being during menopause and beyond.
Looking for ways to enhance your sleep comfort? Discover Sleepgram’s range of pillows, cooling sheets, and comforters designed to help you create your perfect sleep sanctuary. For more insights into achieving better sleep, visit our blog.
